
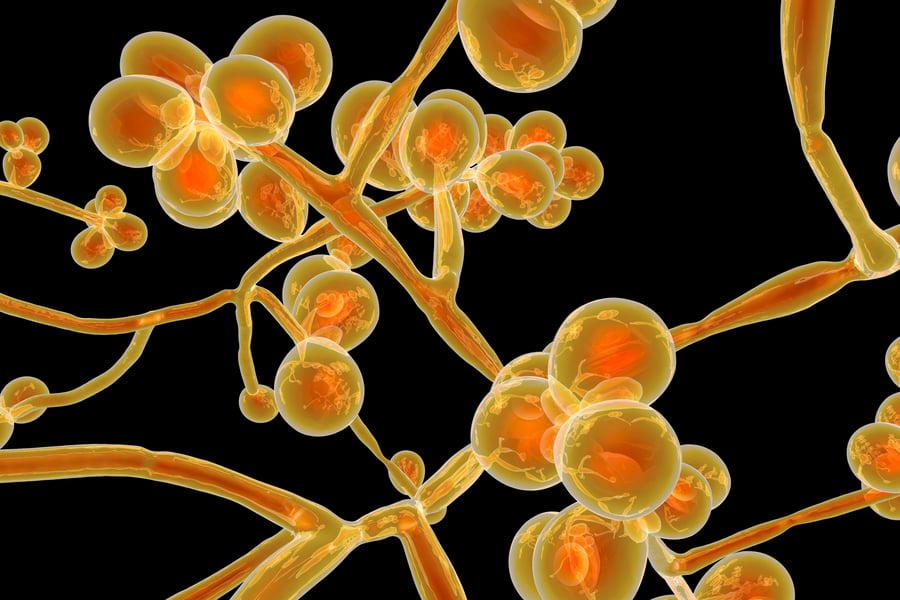
Candida auris: Drug-Resistant Germ Spreading in U.S.
The Centers for Disease Control and Prevention (CDC) is calling Candida auris (C. auris) a “global health threat” as the drug-resistant germ is increasingly responsible for infectious outbreaks in healthcare facilities across the United States.
While still rare in the U.S., the CDC is alarmed by the fact that the fungus leads to bloodstream infections and even death, particularly in hospital and nursing home patients with serious medical problems.
“C. auris is an emerging multidrug-resistant yeast (a type of fungus). It can cause severe infections and spreads easily between hospitalized patients and nursing home residents,” says the CDC.
While named for the Latin word for ear (auris), C. auris can affect many other regions of the body and can cause invasive infections including bloodstream, wound and ear infections.
Special laboratory tests are needed to identify C. auris. which has now spread to over 30 countries and multiple U.S. states, including outbreaks in 2021 in Texas.
The NBC affiliate in Dallas-Fort Worth reported last summer that the “superbug fungus in two Collin County hospitals killed four”.
auris First Identified in 2009, Has Spread Quickly
First identified in 2009 in Japan, C. auris has “become a cause of severe infections around the world” according to the CDC.
A retrospective review of Candida strain collections found that the earliest known strain of C. auris dates to 1996 in South Korea.
Four different strains have reached the United States in recent years:
- South American strain
- African strain
- South Asian strain
- East Asian strain
“Investigators still do not know why four different strains of C. auris emerged around the same time across the globe. All four strains have been found in the United States, likely introduced through international travel and subsequent spread in U.S. healthcare facilities,” says the CDC.
The way it spreads and its resistance to antifungal medications has surprised disease experts.
“It seemed hard to believe. CDC fungal experts had never received a report describing a Candida infection resistant to all antifungal medications, let alone Candida that spreads easily between patients. After hearing the news that infections like this were identified by international colleagues in 2016, CDC sounded the alarm in the United States about C. auris, a life-threatening Candida species,” says the CDC.
auris Symptoms and Those At-Risk
People who get invasive Candida infections are often already sick from other medical conditions, so it can be difficult to know if they have a C. auris infection.
The most common symptoms of invasive Candida infection are fever and chills that don’t improve after antibiotic treatment for a suspected bacterial infection.
Higher Risk candidates for C. auris are patients who have been hospitalized in a healthcare facility a long time, have a central venous catheter, or other lines or tubes entering their body, or have previously received antibiotics or antifungal medications.
Also, people who have recently spent time in nursing homes and have had breathing tubes, feeding tubes and central venous catheters seem to be at higher risk.
Infectious disease experts think these devices can serve as portals of entry for the organism into invasive body sites.
Early research also shows other risk factors could include
- Recent surgery
- Diabetes
- Broad-spectrum antibiotic and antifungal use
- Those with weakened immune systems from conditions such as blood cancers
Infections have been found in patients of all ages, from preterm infants to the elderly.
It should be noted that healthy people usually don’t get C. auris infections.
Treatment of C. auris
Most C. auris infections are treatable with a class of antifungal drugs called echinocandins.
The CDC says that “some C. auris infections have been resistant to all three main classes of antifungal medications, making them more difficult to treat.”
In this situation, multiple classes of antifungals at high doses may be required to treat the infection.
Treatment decisions should be made in consultation with a healthcare provider experienced in treating patients with fungal infections.
7 Things You Should Know About C. auris
auris is an emerging infectious disease and medical research and knowledge is currently being gathered on it. Here are 7 things you should know about C. auris in 2022:- Multidrug Resistant: Some strains are resistant to all three available classes of antifungals commonly used to treat Candida infections.
- Difficult to Identify: Candida auris can be misidentified in labs without specific technology. Misidentification can lead to inappropriate management of the infection.
- Outbreaks in Healthcare Settings: C. auris needs to be identified in hospitalized patients quickly so healthcare facilities can take special precautions to stop its spread.
- Disinfectants Not as Effective: Some common healthcare disinfectants are less effective at eliminating C. auris.
- Spread Without Infection: C. auris can be carried on patients’ skin without causing infection allowing spread to others.
- Causes Serious Infections: C. auris can cause bloodstream infections and even death, particularly in hospital and nursing home patients with serious medical problems. More than 1 in 3 patients with invasive C. auris infection (for example, an infection that affects the blood, heart, or brain) die.
- Becoming More Common: Although C. auris was just discovered in 2009, it has spread quickly and caused infections in more than 30 countries and many U.S. states, including Texas.
Wise Diagnostic Systems offers practical diagnostics to help clinicians achieve better patient outcomes. We are currently working on new testing to help discover....
Subscribe to email updates
Related Articles

Topics

Topics

Topics



